All medical devices that are manufactured in India or are imported into India have to either be licensed or registered by October 1, 2021. If a medical device is manufactured or imported after October 1, 2021 without registration or license, it will be deemed to have been manufactured or imported in violation of Indian law, thereby inviting penal action.
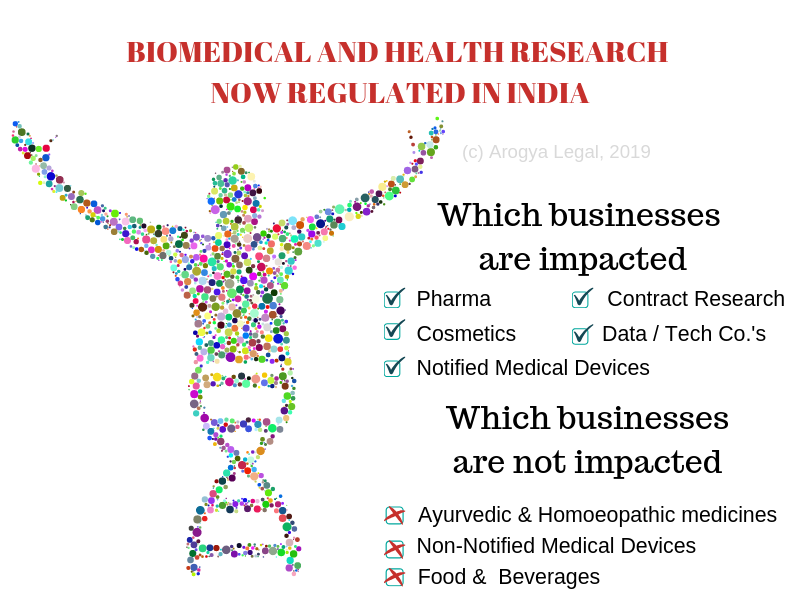
As a background, until 2020, the Indian Government regulated 37 categories of medical devices (scroll down for list) under the Drugs and Cosmetics Act, 1940 (DCA) and Medical Devices Rules, 2017 (MDR) for safety, quality and effectiveness. A license is presently required to manufacture or import these 37 categories of medical devices.
In 2020, the Indian Government brought about a change in law to the effect that manufacturers and importers of all medical devices other than the 37 categories of medical devices have to obtain registration ‘voluntarily’ before October 1, 2021. Those manufacturers and importers who are unable to obtain registration before October 1, 2021 would have to either stop business of said medical devices till they obtain the requisite registration, or risk facing penal consequences of violating DCA and MDR.
With an intent to help and support medical devices companies who wish to obtain a registration, we have put together a list of frequently asked questions (FAQs) with our responses in this article.
Please note that these FAQs are based on our understanding of the law, and under no circumstances should they be regarded as legal or professional advice or an endorsement of any industry practice.
What is this new requirement for obtaining registration for medical devices and equipment?
Owing to an amendment to Medical Devices Rules, 2017 in February of 2020 (said amendment hereinafter referred to as “Medica Devices (Amendment) Rules, 2020” or “MDR 2020”), manufacturers and importers of all medical devices and equipment (with the exception of those that have been notified by the government) in India are required to register their medical devices in India before October 1, 2021.
The list of devices notified by the government, to which the requirement of registration does not apply, is reproduced at the end of these FAQs.
Is the registration requirement voluntary or mandatory?
As per MDR 2020, the enforcement of registration requirementis to begin from October 1, 2021. The government has given time to the medical device industry to register ‘voluntarily’ by October 1, 2021. After that, manufacturers and importers will have to ‘mandatorily’ register their medical devices and equipment in order to be able to manufacture in India or import medical devices into India.
How to obtain registration?
In order to obtain registration, the manufacturer or importer of a medical device or equipment has to register itself, its medical device or equipment as well as the manufacturing site with the Central Drugs Standards Control Organization (CDSCO).
The registration is successful once the file number is generated.
What is the objective behind registration requirement?
The Indian government’s objective behind imposing registration requirement appears to be phase-wise regulation of all medical devices.
The pre-requisite for obtaining registration is just the existence of a ISO 13485 certificate (quality management system for medical devices) issued by a certification body accredited with National Accreditation Board for Certification Bodies (NABCB) or International Accreditation Forum (IAF) to the manufacturer of medical devices. No safety or effectiveness data is required to be submitted for obtaining registration. The intent of the Indian Government appears to be to ensure that by October 1, 2021, all medical devices sold in India must be manufactured at a facility whose quality management systems meet the standards specified in the ISO 13485, as certified by an accredited certifying body.
Is there a list of medical devices available to which the registration requirement is applicable?
CDSCO has published a draft list of medical devices that may require registration. However, since this is only a draft list, there may be medical devices which are not part of the list but would still be subject to registration requirement.
In order to evaluate whether a product qualifies as medical device or not (and consequently would be subject to registration requirement or not), one may refer to the following definition of medical devices under MDR:
All devices including an instrument, apparatus, appliance, implant, material or other article, whether used alone or in combination, including a software or an accessory, intended by its manufacturer to be used specially for human beings or animals which does not achieve the primary intended action in or on human body or animals by any pharmacological or immunological or metabolic means, but which may assist in its intended function by such means for one or more of the specific purposes of ―
(i) diagnosis, prevention, monitoring, treatment or alleviation of any disease or disorder;
(ii) diagnosis, monitoring, treatment, alleviation or assistance for, any injury or disability;
(iii) investigation, replacement or modification or support of the anatomy or of a physiological process;
(iv) supporting or sustaining life;
(v) disinfection of medical devices; and
(vi) control of conception
If a device or equipment is covered by the definition of above, and it is not part of the list of devices specifically notified by the government (see bottom of the article for list), then such a device or equipment will be subject to registration requirement in India.
In certain cases, it may be helpful to avail expert advice in evaluating whether a product or equipment qualifies as a medical device under Indian law and is covered by registration requirement or not.
Whether components and accessories of medical devices are required to be registered?
Component and accessories of medical devices would be subject to registration requirement only if they qualify as medical device as per the definition of medical device i.e. if they are intended by their manufacturer to be used for medical purposes.
As per a recent clarification issued by CDSCO, components and accessories of medical devices imported as a system need not be registered separately. However, it is unclear what ‘separately’ implies, and why such an exemption should be given only to imported systems. It is our view that all components and accessories should be registered as part of the system because the official form for registration has fields under which details of components and accessories may be provided. In case components and accessories are not registered as part of the system for some reason, they should be registered separately, as components and accessories are ‘medical devices’ in their own right as per the definition of medical device.
In other words, components and accessories of medical devices may be registered alongside the system or independently, as long as they qualify as ‘medical device’ as per the definition of medical device.
What are the consequences of not obtaining registration before October 1, 2021?
A device to which registration requirement applies cannot be legally manufactured or imported into India without registration after October 1, 2021. The manufacturers and importers of such medical devices would have to obtain a registration for such devices in India before they can market these devices.
If a device is manufactured or imported after October 1, 2021 into India for marketing purposes without registration, then it would invite penal action under The Drugs and Cosmetics Act, 1940.
Who can make the application for registration?
An importer or manufacturer of the medical device or equipment can make the application for registration.
Can an importer obtain registration for imported medical device or equipment without whole sale drug license?
In order to create an account on the CDSCO’s registration portal as an importer, it is a pre-requisite to possess a whole sale drug license. However, for the time being, CDSCO is allowing registrations without a whole sale drug license as well.
What is the government fee payable for registration?
There is no government fee payable for registration.
What information is required to be provided for obtaining registration?
The following information has to be provided for obtaining registration:
- Legal manufacturer’s name & address with Phone no., Fax & Email id,
- Actual Site Details (Name, Address, Email ID, Fax No. & Contact No.)
- Nature of activity (import/export)
- Category of Device (medical device / IVD)
- Generic Name, Model No.,
- Intended Use,
- Product Description,
- Class of Medical Device
- Medical Device Category
- Grouping Category
- Material of Construction,
- Dimension (If any)
- Shelf Life
- Storage Condition,
- Package Size,
- Sterile or Non-Sterile,
- Brand Name (If registered under the Trade Marks Act, 1999)
What are the documents required to be submitted obtain registration?
In addition to the information, the following documents are required to be submitted for registering a medical device: (1) an ISO 13485 certificate; (2) a Certificate to Foreign Government or Free Sale Certificate (for imported medical devices); and (3) an undertaking stating that the information and documents supplied are true and authentic are required to be submitted.
What is ISO 13485?
ISO 13485 is a standard for quality management system for designing and manufacturing a medical device.
Who issues ISO 13485 certificate?
ISO 13485 certificate is issued by a certifying body. For the purposes of registration, the ISO 13485 certificate must be issued by a certifying body accredited by National Accreditation Board for Certification Bodies in India or the International Accreditation Forum.
What is Free Sale Certificate or Certificate to Foreign Government?
A Free Sale Certificate or Certificate to Foreign Government is issued by a Regulatory Authority / Ministry of the country in which the medical device is approved and marketed. It serves as proof that the medical devices manufactured in the country as freely sold in that country (or region).
Is there a prescribed format for the undertaking to be submitted along with the application?
There is no prescribed format for the undertaking.
What are the compliances to be done after obtaining registration?
The registration number (file number) has to be declared on the label of the medical device.
How long does it take for the registration to be received once the application has been submitted?
After the application for registration is submitted, a file number is generated instantaneously. The generation of the file number concludes the process of registration.
What is the registration number?
The file registration number is the registration number.
Is the registration number different for different medical devices and equipment?
The registration number differs as per the manufacturing site. Different medical device and equipment manufactured at the same site will receive the same registration number. Same medical devices manufactured at different manufacturing sites will receive different registration numbers.
What happens if the applicant submits incorrect information?
Once incorrect information has been submitted, it can only be rectified by CDSCO. The CDSCO requires applicants to submit an undertaking at the time of submission of the application for registration that information contained in the application is true and accurate. Therefore, it is paramount that the information submitted as part of the registration application is true and accurate.
What is the penalty for submitting false information or documents?
The CDSCO may cancel full or part of the registration, effectively making it impossible to sell medical devices in question in India.
Is it possible to sell medical devices and equipment manufactured in India or imported into India before October 1, 2021 without registration?
Given past precedents in similar matters, it is likely that medical devices imported or manufactured before October 1, 2021 may be permitted to be sold in India without registration. However, no medical device imported or manufactured in India after October 1, 2021 may be sold in India if it is not registered and labelled with the registration number.
It will be easy for enforcement authorities to check whether a medical device or equipment has been manufactured or imported into India on or after October 1, 2021 because the Legal Metrology (Packaged Commodities) Regulations, 2011 require the all packaged commodities to contain either date of manufacture or date of import.
Is it possible to sell unregistered medical devices in India which have been manufactured or imported after October 1, 2021?
No. It will be violation of DCA and MDR if a manufacturer, importer or trader sells an unregistered medical device which is manufactured or imported into India on or after October 1, 2021.
In other words, the concerned manufacturer or importer will have to register its medical devices in order to manufacture or import medical devices after October 1, 2021 for sale in India. In such cases, the registration will no longer be “voluntary” but mandatory. The registration number will have to displayed on the label of such medical devices.
Will the process for obtaining registration change after October 1, 2021 when obtaining registration for medical devices and equipment is no longer voluntary?
It is our understanding that it will not change.
For how long is the registration valid?
The registration is valid until appropriate manufacturing or import license is obtained by the concerned manufacturer or importer for those devices.
Before August 11, 2022, importers, manufacturers, distributors, whole sellers and retailers of Class A (low-risk) and Class B (low-medium risk) medical devices will have to compulsorily obtain a license. Before August 11, 2023, importers and manufacturers, distributors, whole sellers and retailers of Class C (medium-high risk) and Class D (high risk) medical devices will have to compulsorily obtain a license. The CDSCO is in the process of undertaking risk classification of all medical devices.
List of medical devices that are not covered by registration requirement
The requirement to obtain registration does not apply to below categories of medical devices as these categories of medical devices are already regulated and require a license for manufacture, import, sale and distribution in India. In other words, if a manufacturer or importer has a license for manufacture or import of medical device, then registration requirement will not apply to such manufacturer or importer.
| 1. Disposable Hypodermic Syringes; | 2. Disposable Hypodermic Needles; | 3. Disposable Perfusion Sets; | 4. Substances used for in vitro diagnosis including Blood Grouping Sera; |
| 5. Cardiac Stents; | 6. Drug Eluting Stents; | 7. Catheters; | 8. Intra Ocular Lenses; |
| 9. I.V. Cannulae; | 10. Bone Cements; | 11. Heart Valves; | 12. Scalp Vein Set; |
| 13. Orthopedic Implants; | 14. Internal Prosthetic Replacements; | 15. Ablation Devices; | 16. Ligatures, Sutures and Staplers; |
| 17. Intra Uterine Devices (Cu-T) | 18. Condoms; | 19. Tubal Rings; | 20. Surgical Dressings; |
| 21. Umbilical tapes; | 22. Blood/Blood Component Bags; | 23. Organ Preservative Solution; | 24. Nebulizer |
| 25. Blood Pressure Monitoring Device | 26. Glucometer | 27. Digital Thermometer | 28. All implantable medical devices Equipment |
| 29. CT Scan Equipment | 30. MRI Equipment | 31. Defibrillators | 32. PET Equipment |
| 33. X-Ray Machine | 34. Dialysis Machine | 35. Bone marrow cell separator | 36. Disinfectants and insecticide specified in Medical Devices Rules, 2017; |
| 37. Ultrasound equipment (effective November 1, 2021) |